
Justin Bellante, a graduate of Dayton Christian High School and former resident of Englewood, is Co-Founder, President and CEO of Atlanta-based healthcare and technology company BioIQ, which recently added antibody testing to its COVID-19 testing platform. (Contributed photo)
As many stay-at-home orders have lifted across the country, the idea of going back to health before going back to work has become pivotal to the national COVID-19 discussion. Among those fighting for the growing need to accelerate widespread testing is Justin Bellante, Co-Founder, President and CEO of Atlanta-based BioIQ.
“How do you get people back to work? We liken it to after 9/11,” said Bellante, a Dayton Christian High School graduate formerly of Englewood. “After 9/11 no one wanted to get on an airplane. And it wasn’t until the TSA was created and so much testing, measurement and screening was (implemented) at airports that enough confidence was provided to the general public that it was safe to get on an airplane again. So, when you think about going back to work it’s really analogous to that. Are we going to, as private employers or public society or governments, start to create an infrastructure and framework where we feel it’s safe to go back to work? And, of course, the most important thing is testing. So, in an ongoing way, you have to know if you’re safe in that environment. The cornerstone of a back to work program has to be ongoing assessment and contact tracing, which has been validated in South Korea and other countries as the recipe to manage the virus until we learn more or develop a vaccine.”
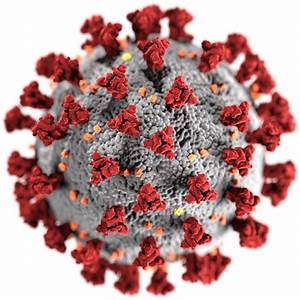
 Founded in 2005 in Santa Barbara, California, BioIQ, a healthcare engagement and clinical adherence technology platform company, recently added antibody testing to its numerous COVID-19 initiatives, including saliva RT-PCR diagnostic testing, for health plans, employers and government agencies. The company is particularly conducting quantitative antibody testing, which is done in a laboratory on a large clinical analyzer with an accuracy of 95 percent or more, according to Bellante.
Founded in 2005 in Santa Barbara, California, BioIQ, a healthcare engagement and clinical adherence technology platform company, recently added antibody testing to its numerous COVID-19 initiatives, including saliva RT-PCR diagnostic testing, for health plans, employers and government agencies. The company is particularly conducting quantitative antibody testing, which is done in a laboratory on a large clinical analyzer with an accuracy of 95 percent or more, according to Bellante.
“The RT-PCR test (determines) whether or not someone currently has the virus,” he explained. “The antibody test is more downstream. It determines if someone previously had the virus and if their body produced antibodies to fight the virus. Antibodies last for a long period of time. What’s so interesting about this is we think over time that being able to do two of those antibody tests will help us understand if someone is immune to the condition. Meaning, those are people we would value in society because they can’t get the virus again. But epidemiologists and virologists don’t know right now if you can get it again. Is this like the common cold, which you can catch every couple of months? Or is it like the flu, which you can get for one season, you fight it, and your body builds immunity to that strain until the following flu season when the flu mutates. We don’t know if the coronavirus is going to mutate. Season by season, is it going to be treated the way we treat the flu now? Or can your body even develop enough immunity? There have been cases recently in South Korea in which people had coronavirus, recovered, and two months later got it again. Because testing wasn’t available across the U.S., a lot of people probably had it or think they had it and now they want to know if they had it. It’s too late to do the PCR testing because the virus has probably left their bodies but the antibody testing will tell them if they had it.”
Bellante, who holds a bachelor’s degree and a master’s degree in materials engineering from Case Western Reserve University, also endeavors to bring the company’s initiatives to people on a wider scale. For example, there can be noticeable contrasts between labs with testing capacity in Arizona versus labs in New York lacking capacity.
 “Even if you have testing available, it doesn’t mean you’re testing people,” he said. “We’re really focused on leveraging our technology platform to get testing capacity to the people that need them. You have to have workflows to get tests to hospitals, screening tents and critical infrastructure workers at their place of work such as a factory or retail distribution center. Creating workflows to get testing to people is the major challenge. And even in COVID-19 testing, we’re already starting to see disparities and outcomes between different racial, ethnic and socioeconomic groups who are being more impacted.”
“Even if you have testing available, it doesn’t mean you’re testing people,” he said. “We’re really focused on leveraging our technology platform to get testing capacity to the people that need them. You have to have workflows to get tests to hospitals, screening tents and critical infrastructure workers at their place of work such as a factory or retail distribution center. Creating workflows to get testing to people is the major challenge. And even in COVID-19 testing, we’re already starting to see disparities and outcomes between different racial, ethnic and socioeconomic groups who are being more impacted.”
With mid-April statistics indicating roughly 3.2 million COVID-19 tests have been conducted across America, which accounts for about 1 percent of the total U.S. population, Bellante is aware of the long road ahead. However, with guidance from a Public Health Advisory Board including Regina Benjamin, the 18th U.S. Surgeon General, he is grateful for the insightful perspectives allowing the company to thrive while helping to save as many lives as possible.
“We are in a crisis,” he said. “This is a pandemic. There are a lot of unknowns in this unprecedented situation. This isn’t going to go away May 1 or May 15 and the world is going to go back to normal. We’re more than likely going to deal with this situation for many months to come. We have to have urgency but not be in emergency mentality. We have to have urgency but we have to be thoughtful.”